Customer Engagement & Experience for Payers
Elevating Customer Interactions, One Insight at a Time.
AI-Powered Analytics to Enhance Satisfaction, Retention, and Reputation.

Transforming Engagement with AI-Powered Insights
For healthcare payers, customer engagement is the cornerstone of retention and profitability. Delays in service or negative experiences can lead to rapid churn and a loss of brand loyalty.
DeepForrest’s Customer Experience Analytics (Cˣ) Platform empowers payers to deliver personalized experiences, foster loyalty, and gain actionable insights across the customer lifecycle.

Benefits
- Increased Customer Satisfaction
- Enhanced Retention with Proactive Solutions
- Improved Brand Reputation and Trust
- Real-Time Feedback and Insights
- Competitive Differentiation
- Reduced Churn through Proactive Engagement
- Data-Driven Decision Making for Better Outcomes
AI-Driven Customer Experience Analytics Platform - Cˣ
Proactively engage with patients throughout their journey to build long-term loyalty:
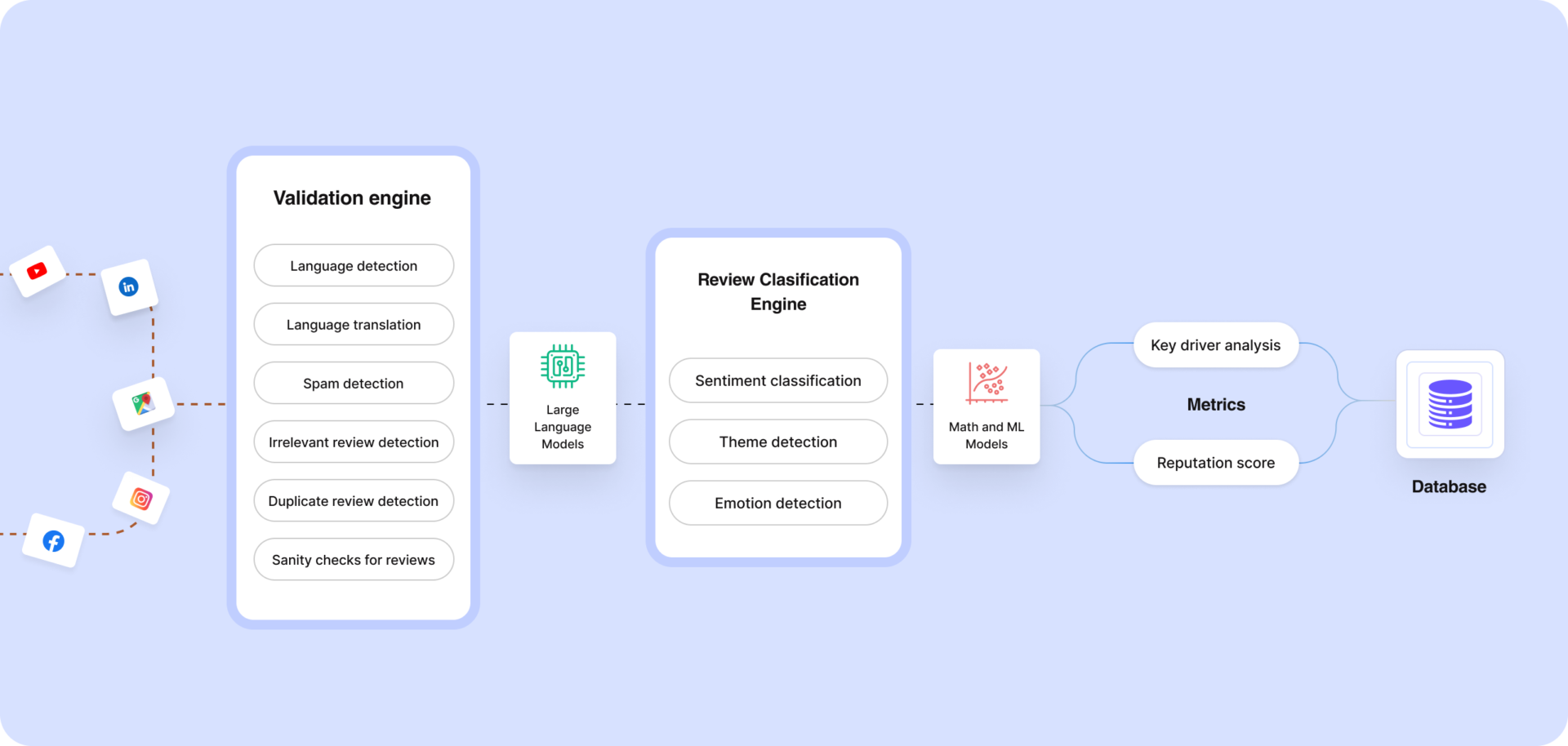
Multichannel Feedback Integration
Consolidate feedback from surveys, social media, call centers, and other channels to create a unified, 360-degree view of customer sentiment.
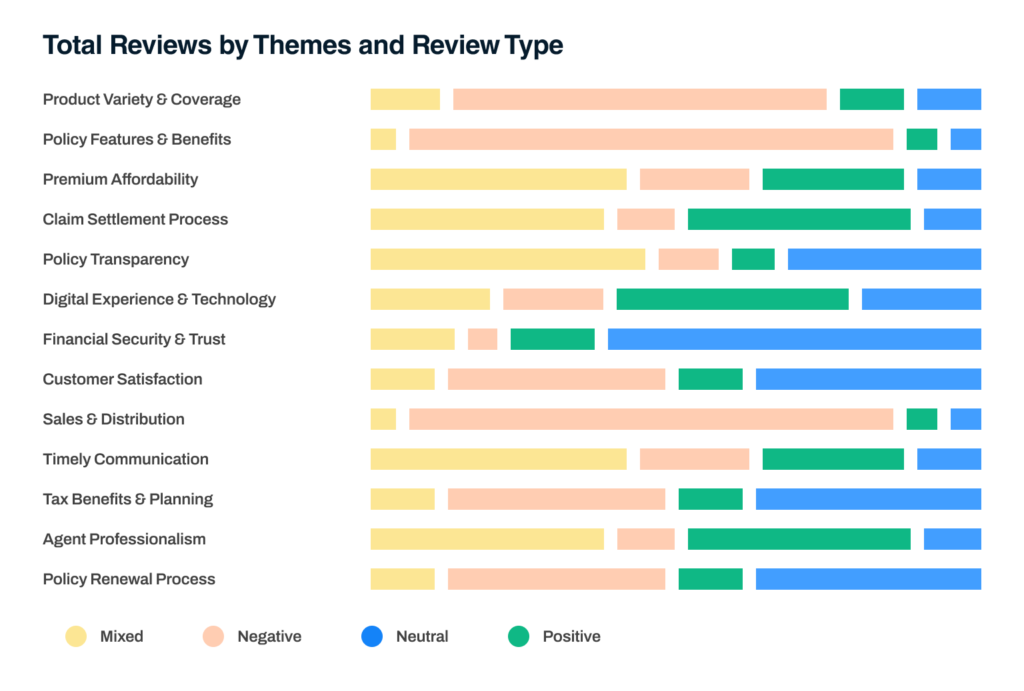
Sentiment Analysis
Understand customer emotions and concerns by analyzing feedback across multiple channels.
Themes & Sub-Themes Identification
Extract meaningful themes and sub-themes from feedback to uncover key trends and focus areas.
Key Drivers
Pinpoint the factors influencing satisfaction, loyalty, and churn to target specific improvements.
Reputation Score
A comprehensive metric that aggregates feedback across channels to reflect brand perception and customer trust.
Industry Benchmarking
Compare your organization’s performance against industry standards to identify opportunities for growth.
Customer Loyalty Score
Measure and track customer loyalty to refine engagement strategies and strengthen relationships.
Customer Touch Point Score
Evaluate performance at each touchpoint to ensure a seamless and satisfactory customer experience.
Negative Feedback Alerts
Proactively address dissatisfaction by identifying and mitigating potential issues before they escalate.
Department Scores
Assess and improve the performance of individual departments to deliver consistent quality across the organization.
Competitive Intelligence
Gain insights into competitor weaknesses and market opportunities to enhance your positioning and strategies.
Impact on Revenue
Quantify the financial benefits of improved customer satisfaction, loyalty, and operational efficiency, linking better engagement to measurable outcomes.
Empowering Healthcare Payers to Lead with Customer-Centric Strategies
Payers often face challenges such as customer churn, negative experiences during claims, and a lack of actionable insights. With our Cˣ platform, these challenges turn into opportunities.
Enhancing Customer Engagement & Experience:
Social Media Monitoring
Track and respond to customer feedback on platforms like Facebook and Twitter to protect and enhance your reputation.
Feedback Alerts
Quickly identify and address issues to prevent dissatisfaction from escalating.
Customer Loyalty Score
Measure and improve loyalty through personalized campaigns and engagement.

Driving Better Business Outcomes
Increased Retention Rates
Retain more customers with a 360-degree view of their interactions and preferences.
Feedback Alerts
Use AI to reduce manual effort and operational costs while enhancing customer satisfaction.
Improved Customer Acquisition & Revenue Growth
Attract new customers by highlighting strengths in service quality and responsiveness.
Social Reputation Score:
Redefining Customer Trust
DeepForrest’s Social Reputation Score provides a comprehensive, AI-driven assessment of your brand’s perception, enabling healthcare payers to proactively manage and enhance customer trust and loyalty. It is an accurate reflection of customer satisfaction and brand health.
What is the Social Reputation Score?
The Social Reputation Score is an advanced, AI-calculated metric that measures how your brand is perceived across multiple feedback channels, including:
Social media platforms (Facebook, Instagram, Twitter, etc.)
Online reviews (Google Reviews, Yelp, etc.)
Internal and external surveys
Voice of the customer (VOC) programs
Unlike traditional measures like Net Promoter Score (NPS) or star ratings, the Social Reputation Score offers a holistic and actionable view by consolidating and normalizing feedback across various touchpoints.
Why Social Reputation Score Matters
Build Trust and Retain Customers
89% of customers trust online reviews as much as personal recommendations. A strong reputation can significantly reduce customer churn and foster long-term loyalty.
Improve Customer Acquisition
Positive sentiment attracts new customers. A higher reputation score positions your brand as a reliable and customer-centric choice.
Mitigate Risks
Identify and address negative feedback trends early to avoid potential PR crises that can damage trust and profitability.
Boost Profitability
A 5% increase in customer retention can lead to a 25-30% boost in profitability, directly tied to reputation management.
Why choose us?
Our AI solutions enable healthcare payers to optimize operations, reduce costs, and enhance member experiences.

Healthcare Domain Expertise
With a deep understanding of healthcare’s regulatory and operational landscape, we design solutions that meet industry standards.

Domain Specific AI Models
Using state-of-the-art domain specific models, from Large Language Models (LLMs) to predictive ML models, we offer advanced solutions that are as reliable as they are innovative.
Outcome oriented approach
Our solutions yield tangible results, from reducing missed appointments to increasing patient satisfaction and retention, reducing processing times, improved clinical outcomes.

AI Maturity assessment
AI readiness assessments that map the customer journey, identify high-ROI use cases, and build a roadmap for implementation.

HIPAA, GDPR, FDA Compliant solutions
Our solutions are built with compliance at their core, ensuring adherence to HIPAA for data privacy, GDPR for global data governance, and FDA standards for safe, effective AI tools.

Explainable and Trustworthy AI
Easy to understand for clinicians, underwriters, with robust AI governance and AI guardrails in place.
Whether it's claims management, fraud prevention, or operational efficiency, we bring innovation and excellence to every aspect of your business.
Success Stories: AI & Analytics Transforming Insurance

85% reduction in processing time, increased accuracy, and enhanced focus on higher-value tasks.
Ready to Redefine Customer Experience?


