Claims Processing and Automation
AI-Driven Solutions to Automate Workflows, Reduce Processing Time, and Boost Operational Efficiency.

We Streamline Claim Workflows with Advanced Automation
Efficient claims processing is no longer a back-office task. It’s a strategic lever for profitability and customer satisfaction.
Delays and errors in claims management cost healthcare payers billions annually and negatively impact member retention.


Faster Claim Resolution

Improved Accuracy

Enhanced Customer Experience

Cost Efficiency

Regulatory Compliance

Reduced Operational Costs
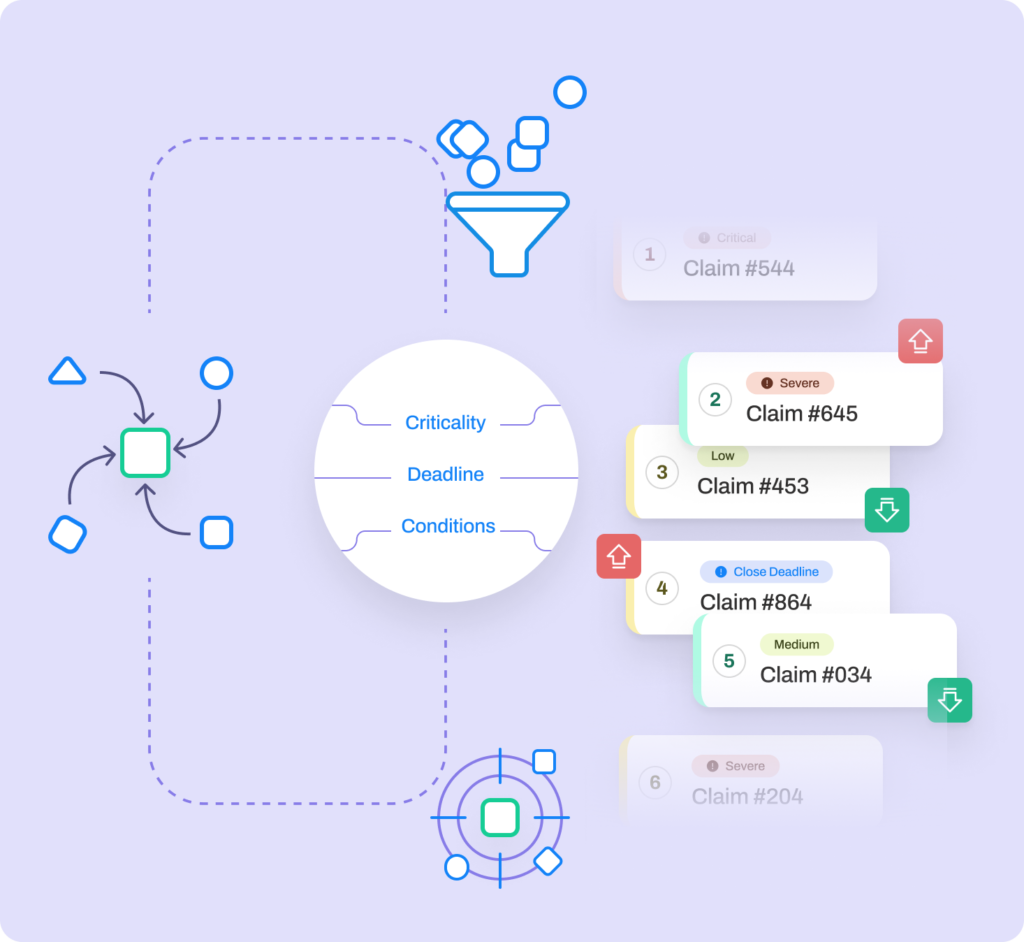
Our AI-driven solutions revolutionize claims management by automating repetitive tasks, improving accuracy, and reducing processing time.
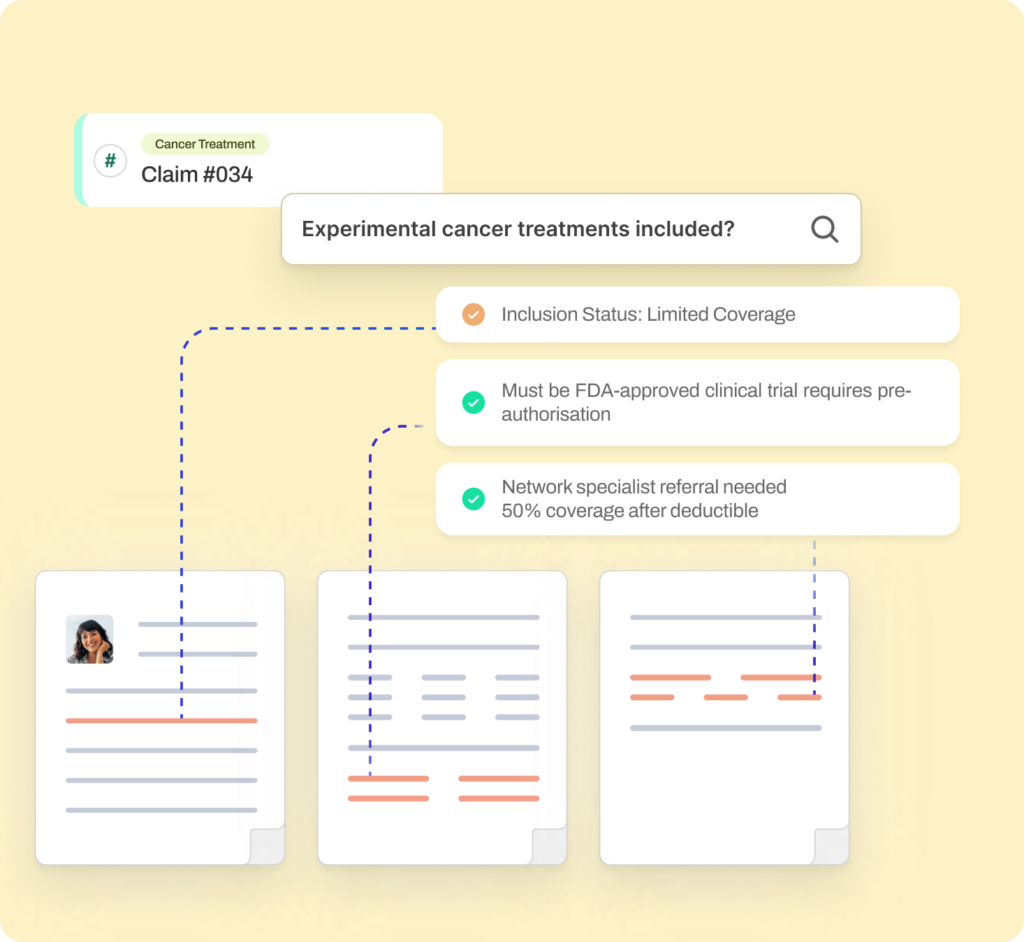
AI-Driven Claim Admissibility Process Automation
Traditional claims processing is often hindered by manual steps and data handling. Our AI-powered solution simplifies the process.
Document Identification and Classification
Accurately categorize and verify documents using LLMs trained on historical claims data.
Data Extraction for Claim Admissibility
Extract critical details from unstructured documents and cross-check them against admissibility criteria.
Real-Time Summaries and Status Updates
Deliver actionable insights through dashboards, ensuring compliance and transparency.
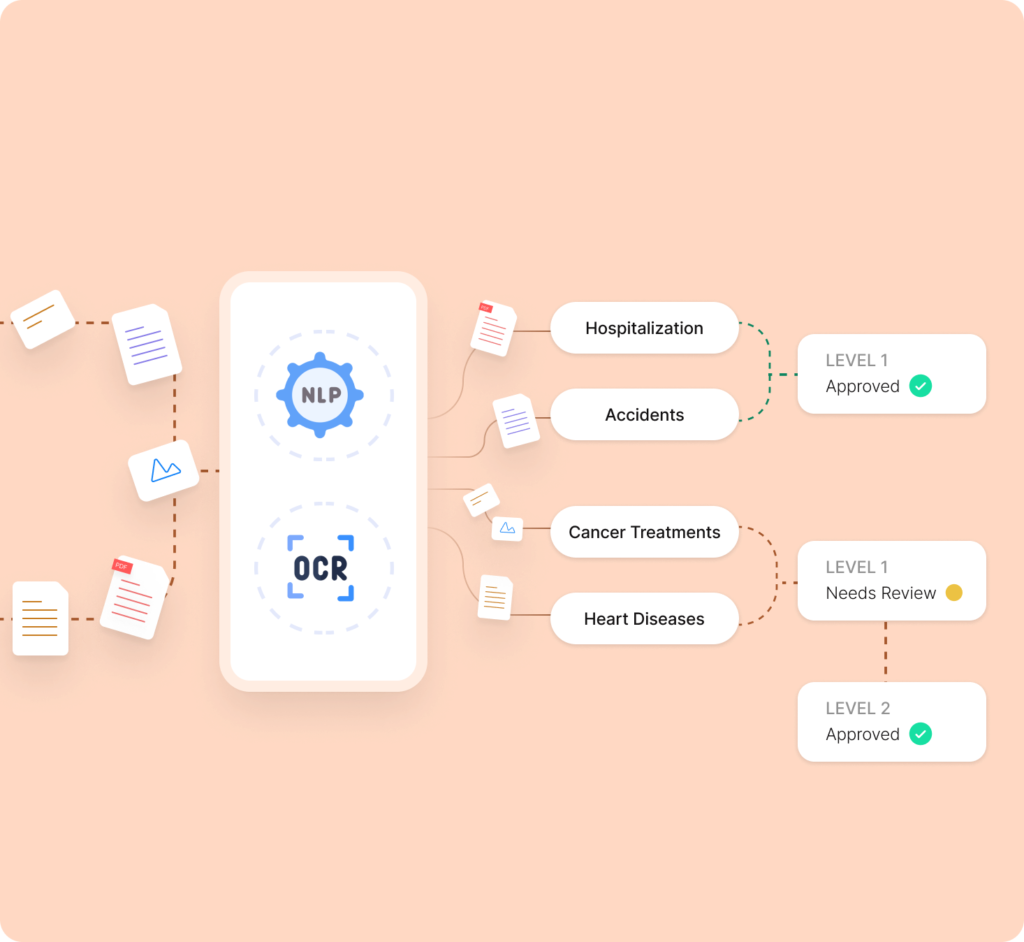
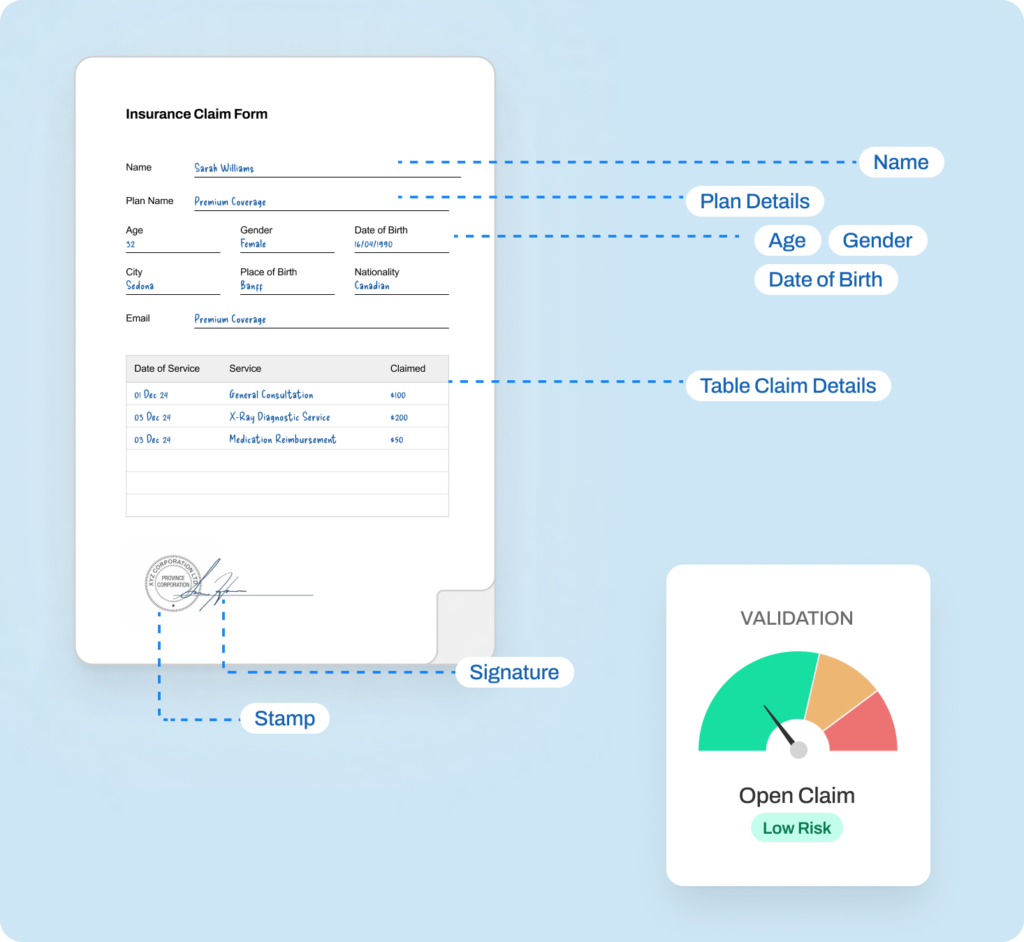
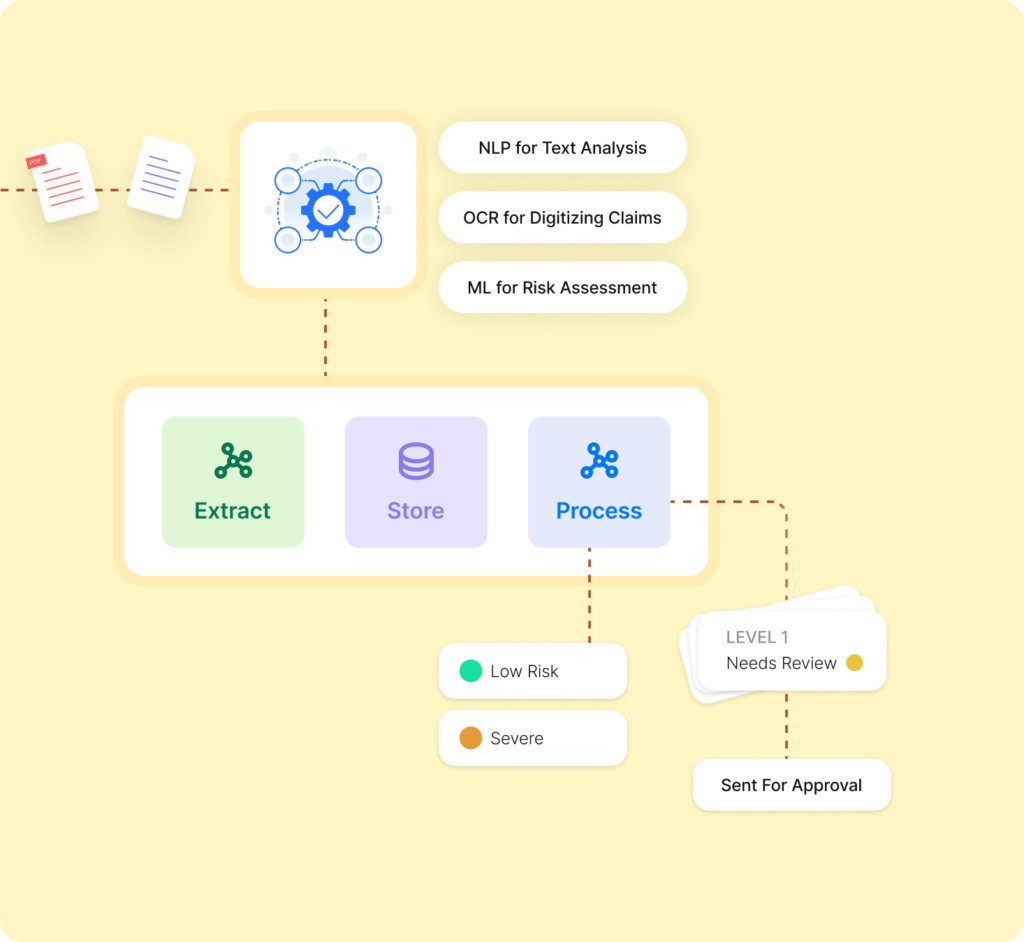

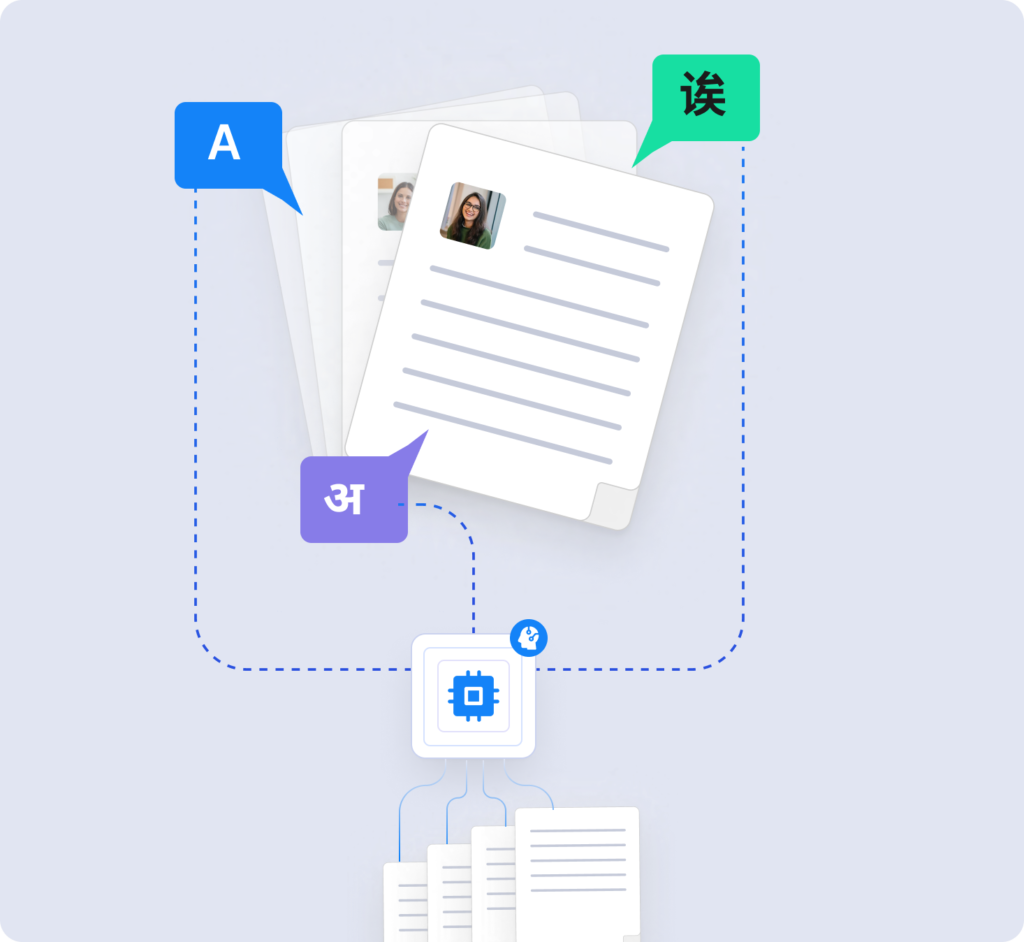
Auto Abstraction of Data Elements with NLP-Driven Automation
Our Auto Abstraction of Data Elements solution leverages advanced Natural Language Processing (NLP) to extract, classify, and structure information from unstructured documents.
This not only improves operational efficiency but also ensures accuracy across clinical, billing, and regulatory workflows.
Clinical Documentation Improvement
Automatically extract critical clinical information from unstructured notes, enhancing the accuracy and completeness of patient records.
Regulatory Compliance and Reporting
Streamline reporting to regulatory bodies by automating the extraction and structuring of data for compliance with standards like HIPAA and PIPEDA, as well as other quality reporting requirements.
Billing and Coding
Extract relevant billing data from clinical notes to ensure accurate coding of procedures. This reduces billing errors, enhances revenue capture, and mitigates audit risks.
Operational Efficiency
Automate repetitive data extraction tasks, reducing the administrative burden on healthcare professionals and allowing them to focus on patient care.
Why choose us?
Our AI solutions enable healthcare payers to optimize operations, reduce costs, and enhance member experiences.

Healthcare Domain Expertise
With a deep understanding of healthcare’s regulatory and operational landscape, we design solutions that meet industry standards.

Domain Specific AI Models
Using state-of-the-art domain specific models, from Large Language Models (LLMs) to predictive ML models, we offer advanced solutions that are as reliable as they are innovative.
Outcome oriented approach
Our solutions yield tangible results, from reducing missed appointments to increasing patient satisfaction and retention, reducing processing times, improved clinical outcomes.

AI Maturity assessment
AI readiness assessments that map the customer journey, identify high-ROI use cases, and build a roadmap for implementation.

HIPAA, GDPR, FDA Compliant solutions
Our solutions are built with compliance at their core, ensuring adherence to HIPAA for data privacy, GDPR for global data governance, and FDA standards for safe, effective AI tools.

Explainable and Trustworthy AI
Easy to understand for clinicians, underwriters, with robust AI governance and AI guardrails in place.
Whether it's claims management, fraud prevention, or operational efficiency, we bring innovation and excellence to every aspect of your business.
Success Stories: AI & Analytics Transforming Insurance

85% reduction in processing time, increased accuracy, and enhanced focus on higher-value tasks.
Set to Redefine Claims Efficiency?


